In 2018, Mike Ferraro was living on the street and sharing needles with other people who injected drugs when he found out he was HIV-positive.
“I thought it was a death sentence, where you have sores and you deteriorate,” he said.
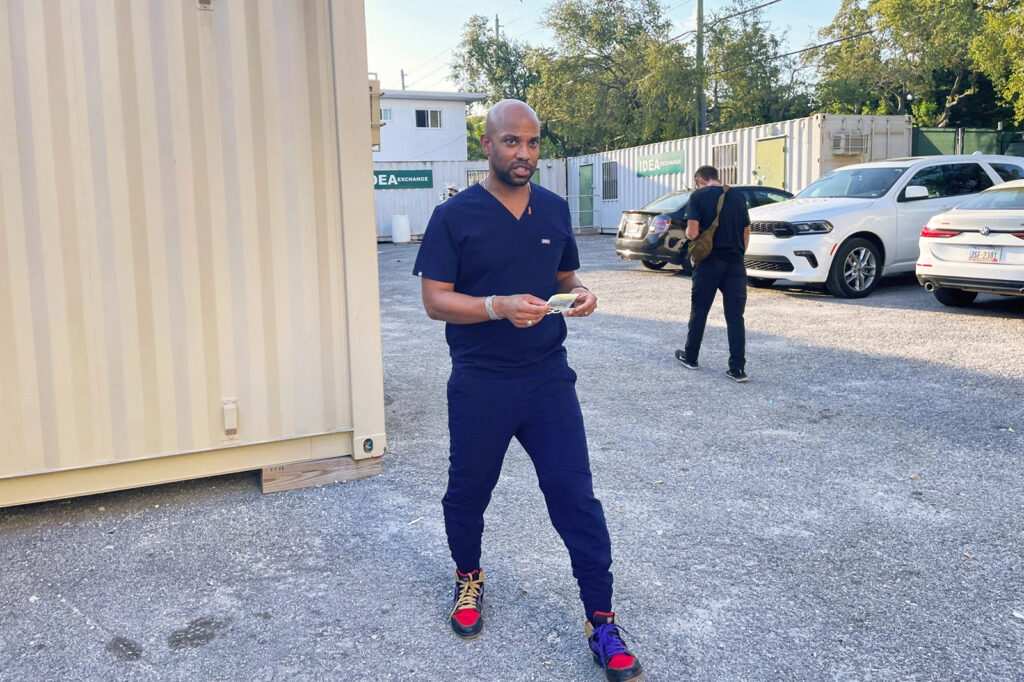
Ferraro learned of his HIV status through a University of Miami Miller School of Medicine initiative called IDEA Exchange, which sent doctors and medical students to the corner where he panhandled. He got tested and enrolled in the program, which also provides clean syringes, overdose reversal medications, and HIV prevention and treatment drugs.

Under normal circumstances, it could have taken months for Ferraro to get on viral suppression medication, if he got on it at all. But the same day he learned his status, an IDEA Exchange doctor started Ferraro on a drug regimen.
His HIV is now in check, and he is recovering from drug use. “They save lives,” said Ferraro, now 55, adding that he was treated with kindness and respect and didn’t feel stigmatized, which encouraged him to enter treatment.
Launched in 2016, IDEA Exchange practices a new approach to treating and preventing HIV infections that combines telehealth with direct outreach, aided by more than $400,000 in grants from the Centers for Disease Control and Prevention and other federal agencies. The funding is part of a national effort launched by the White House in 2019, under former President Donald Trump, called Ending the HIV Epidemic in the U.S.
The federal initiative aims to cut the number of new HIV infections nationwide by 75% by 2025 and 90% by 2030. Officials hope to achieve those milestones by funding new, community-specific strategies to deliver care to hard-to-reach groups, such as people who inject drugs, and others who are living with or at risk of contracting HIV.
Federal health agencies have sent hundreds of millions of dollars to cities, states and territories hit hardest by the epidemic — many in the South. Georgia, Louisiana, and Florida were among the states with the highest rates of new HIV diagnoses in 2020, according to the CDC.
But people living with HIV, doctors, infectious disease experts, community groups and some of the nation’s top HIV officials say the initiative could miss its main 2030 goal.
“Do I think the whole country is going to make it there? I don’t think so,” said Harold Phillips, head of the White House Office of National AIDS Policy.
The COVID-19 pandemic, workforce shortages and bureaucratic red tape have slowed HIV response efforts. And local programs have been hobbled in places where stigma and discrimination are fanned by anti-LGBTQ+ messaging from elected officials, especially in states where legislators have proposed restrictions on health care, education and drag shows.
“We all were not at the same starting point,” Phillips said.
Because of pandemic disruptions, federal officials haven’t had solid estimates of new infections or the number of people living with HIV since the end of 2019, Phillips said. The available data suggests the goal of dramatically reducing new infections is a long way off. HIV testing and uptake of preventive drugs, such as preexposure prophylaxis, or PrEP, and viral suppression medications are also falling short.
The White House hopes to have more accurate data this year that will allow officials to adjust HIV response efforts to make up lost ground, Phillips said.
Since 2019, Congress has incrementally increased spending on the program’s efforts to prevent HIV — it’s $573 million for the current fiscal year — but has repeatedly provided less than what Trump or, later, President Joe Biden requested. Now, with Republicans angling for steep budget cuts, Biden’s current request for $850 million stands on shaky ground.
But even as the administration seeks more money, state and local public health officials have been unable to spend all the hundreds of millions they’ve been granted.
KFF Health News contacted several counties and states in February to ask how they spent money from the U.S. Department of Health and Human Services meant for ending the HIV epidemic. Kentucky, South Carolina and Arkansas had spent less than half of their allocations. And county officials in DeKalb County, Georgia; Harris County, Texas; and Mecklenburg County, North Carolina, said they had also yet to spend all their Ending the HIV Epidemic funding.
Those dollars have to be spent within county lines, which reduces their impact in outlying parts of the metro area, said Matt Jenkins, director of the HIV/STD division of Mecklenburg County Public Health in Charlotte.
And requirements that contracts over $100,000 go through a “labor-intensive” bidding process and that final spending decisions receive state approval also act as roadblocks, Jenkins said.
Such administrative processes can make it harder for federal money to reach local HIV service providers that target previously unreached communities. Instead, Jenkins said, funding tends to flow to well-established groups that may crowd a community with the same type of service, like more locations for testing.
“Is that new and innovative? No,” he said.
While officials like Jenkins navigate bureaucratic and logistical problems, some HIV programs also face decades-old political and ideological obstacles.
This is the case in Tarrant County, Texas, said Hope Adams, manager for the local Ending the HIV Epidemic program. Leaders there hesitate to acknowledge that HIV disproportionately affects marginalized groups such as gay and bisexual Black and Hispanic men, Black heterosexual women and transgender people.
“If you deny that systemic discrimination exists, then you’re not going to want to fund programs that say, ‘Hey, we need to focus on disadvantaged populations,’” she said.
That mindset also limits how her agency can reach people, Adams said. She’d like to promote services on dating apps like Grindr and Tinder but said she’s allowed to use only “the safe ones”: Facebook, Twitter and Instagram.
“Our messaging has to be conservative. It has to be very delicately phrased. You can’t have an image of a condom, for example,” she said. “It affects us in terms of getting our message out in a way that connects with people and to the right audience.”
Acknowledging structural problems can get officials labeled as “woke,” injecting politics into public health and undermining progress — despite the scientific advances made in treating and preventing HIV.
Like the COVID-19 pandemic, the HIV epidemic has highlighted long-standing social and economic inequities, which reduce access to care.
Though most people with private insurance do not pay out-of-pocket for PrEP and related doctor visits and lab tests, that may change, pending the final outcome of a legal challenge to an Affordable Care Act mandate that most private insurance plans cover recommended preventive care services. Overturning the requirement could make preventive HIV care unaffordable for many people.
Mitchell Warren, executive director of AVAC, a global HIV advocacy group, pointed also to other social challenges, such as lawmakers across the U.S. targeting gender-affirming care, drag shows, and diversity, equity and inclusion programs. Politics — and pressure from conservative activists — recently led the state of Tennessee to turn down more than $8 million in federal funding to fight HIV.
“We often think HIV is about condoms and antiretroviral therapy and PrEP,” Warren said. “It is. But those products only help people if they can go into a facility where they are treated with respect, with high-quality care, where they’re not worried that the clinic is going to get bombed or closed down in controversy.”
The White House’s Phillips, an openly gay man living with HIV, acknowledged the current “tough environment” and said he remembered “the days when HIV had bipartisan support.”
He hoped that elected officials could find that common ground again, recognize the value of HIV prevention, and continue to invest in it — even beyond the 2030 deadline.
Ending the epidemic will require sustained funding and political will, which can be threatened regardless of whether a program misses its mark or shows signs of success, said Bernard Davis, president of RAO Community Health, a clinic in Charlotte.
“When you begin to see the outcomes looking better than they did before, you then remove those dollars,” he said. “Well, the community goes back to where it was from the beginning, because those resources are no longer there.”
___
© 2023 Kaiser Health News
Distributed by Tribune Content Agency, LLC.



